Editor’s Note: Mary Kitchell, one of the incumbents, is married to Ames Voice reporter Michael Kitchell.
For Ames residents, it’s the one contested office on the 2025 election ballot. Ames’ hospital Board of Trustees has two incumbents and one challenger running for two seats.
While Mary Greeley Medical Center has an administrative team that operates the city-owned hospital on a day-to-day basis, the trustees are responsible for tasks such as managing and governing the hospital as well as managing funds, negotiating charity care, authorizing delivery of health services and budgeting for hospital improvements and maintenance.
The Voice sent questions to all three candidates to find out who they are, what their background is and Mary Greeley’s successes and challenges.
The general election is Nov. 4. Find out your polling place here, register to vote online, find out who else is up for election here and keep up with Story County election information right here at the Ames Voice.
City Hospital Trustees
Voters will select two on the ballot for hospital trustees.
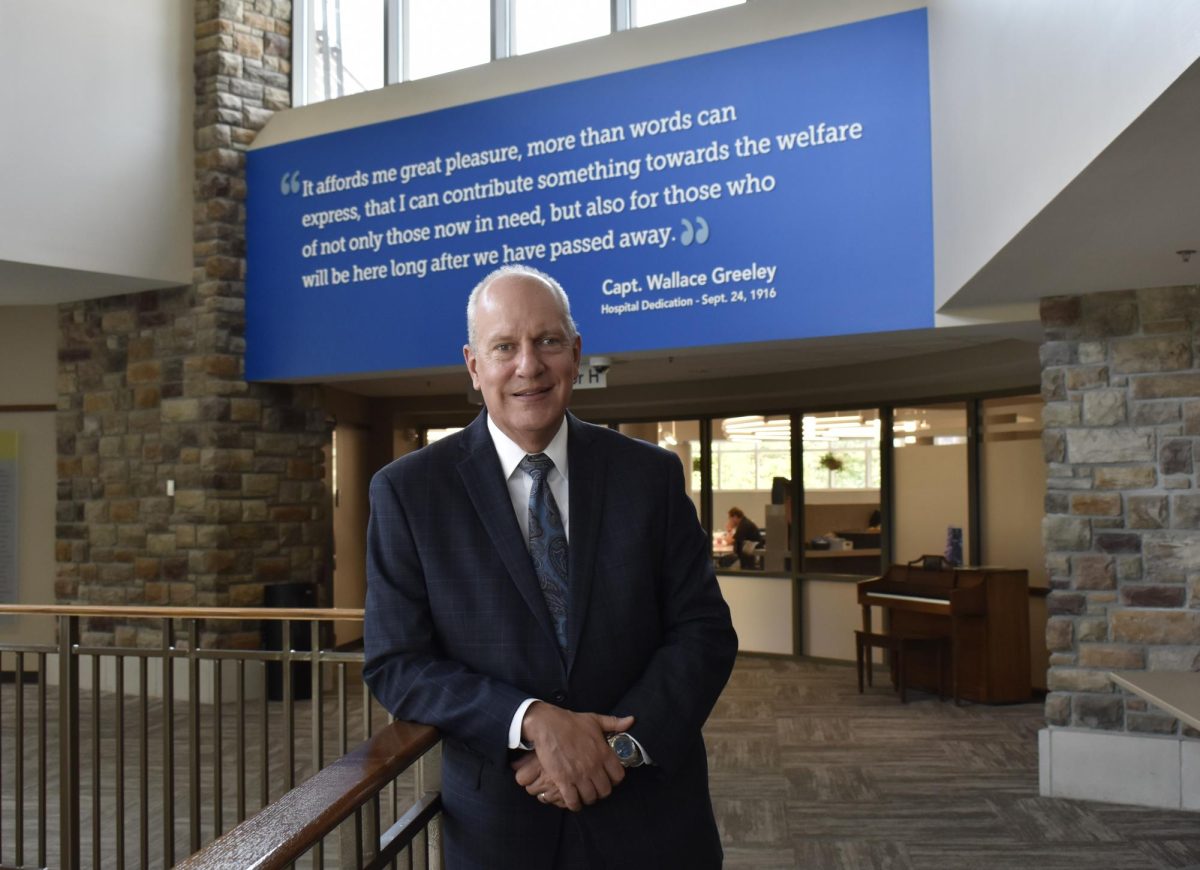
Paul Hudson
Years in Ames: 60 years (my family moved here when I was in kindergarten)
Day job: Retired. I travel frequently and extensively and have just returned from a trip that moved my country count to 50. I’ve visited all seven continents.
What, if any, background do you have in health care? As an undergraduate at Iowa State, I took a CPR class, then a CPR instructor class, then an EMT-A class, then Mary Greeley Hospital’s first paramedic program. I was hired by the hospital during that class, then helped teach the second and subsequent classes, along with a wide variety of classes for the public, volunteer and paid professionals. I became a paramedic supervisor and worked at mobile intensive care services for over 20 years. After a year of work for Managed Healthcare Services I returned to EMS as a flight paramedic — first with Mercy AirLife in Mason City, then with LifeFlight in Des Moines.
I went back to school for an MBA at Iowa State and then a Masters in Healthcare Administration at Des Moines University. I became a Fellow of the American College of Healthcare Executives and served on the board of directors for the Emergency Department Practice Management Association for 15 years, and continue to serve on committees.
I joined Acute Care, Inc., a physician practice that recruits, credentials and schedules emergency physicians at over 40 small, rural hospitals in six states, as a vice president and then chief operating officer. I helped the practice grow and mature over my 21 years at what became STATUS Healthcare Partners, and gained experience in contract management, strategic planning, operations, customer and patient care, quality improvement, and mergers and acquisitions.
I’ve lectured state-wide and nationally on a variety of topics, with a focus on resuscitation, patient satisfaction, and rural emergency care. I served as national and regional faculty for the American Heart Association’s Advanced Cardiac Life Support (ACLS) and Pediatric Advanced Life Support (PALS) programs. I was selected as a National Examiner for the Malcolm Baldrige National Quality Award Program, and served for three years.
What led you to run for the board? I worked with Sarah Buck at MGMC, and when I received notice that she’d retired as chairperson of the board, I approached Mr. Dieter with word of my interest. He and the current chairperson, Ken McCuskey, were kind enough to meet with me and hear my story and my motivation to join the board — that I believe my education, experience and appreciation of the contribution of the hospital and its standing relative to other health systems I’ve examined leads me to believe that I am ideally suited to give back a portion of the benefits that I’ve been accorded as an employee, patient and member of the community. I was told board positions were all filled and the next election would be in a year and a half. They offered, and I accepted, a position as community member in the strategic planning process. I attended the board meetings as a visitor and participated in all strategic planning sessions.
Mary Kitchell

Years in Ames: 45 years
Day job: Retired. Previously I worked part-time as a provider at Ames Counseling and Psychological Services. I have B.S., M.A., and Ed.S. degrees in psychology. I have also devoted considerable time to volunteer service in a variety of community organizations through direct participation and leadership roles.
Board of trustees member: 25 years
What, if any, background do you have in health care? I began my professional career as a consultant at the University of Iowa Department of Pediatrics engaging in direct patient care, teaching, and research. I have been married for almost 50 years to a physician and understand the life experiences and challenges that physicians face. At the state level, I serve on the Iowa Medical Society Foundation board and have been formally recognized by the IMS as a “champion of Iowa physicians.” In 1998 I co-founded the Ames Free Medical Clinic and served as its administrator for 16 years. I served on the team that successfully applied for the establishment of a Federally Qualified Health Center in Ames. At Mary Greeley, I have served in a variety of volunteer positions, including leadership as the Auxiliary Board Chair and the Foundation Board Chair. To this day, I work as a volunteer courier at the hospital front desk where I help patients navigate the hospital corridors, gaining understanding of their experiences and the work of the staff. At the Iowa Hospital Association, I maintain Hospital Trustee Education Certification and also serve on the IHA Legislative Policy Council. I received the “Excellence in Governance” award from the IHA. At the American Hospital Association, I have served on five different advisory committees. The state and national organizations have provided a broadened understanding of health care, introduced me to best practices, and helped me make informed decisions. I have been recognized in the Ames community by United Way, YSS, Ames Chamber, Ames Tribune, YWCA and the Iowa Volunteer Hall of Fame for my efforts in health care.
What led you to run for the board? I was asked to fill a vacant seat mid-term, and subsequently, I have been encouraged to continue by those with whom I work. I find the work on the board challenging and meaningful.
Beth Swenson

Lived in Ames: 39 years
Day job: Retired
Board of trustees member: since 2018
What, if any, background do you have in health care? I have worked in health care as a medical technologist for over 40 years, with 28 years at Mary Greeley. While employed there I served on the employees action committee and was the employee representative on the search committee for a new president (Jeff Stevensen). I also served on the employee United Way committee. As a board member, I’ve served on the finance, patient and family advisory, and quality and safety committees. I’m currently the chair of the human relations committee.
What led you to run for the board? One of my motivations to serve on the board is to be a representative of the employees. I approach every decision with “How will this affect the employees?” Employees who are valued and respected play a critical role in contributing to MGMC’s reputation as a high quality, safe place to receive care with a personal touch. I have learned a great deal during my eight years on the board and look forward to four more years. I want to continue to work to keep our hospital the great place it is!
What are MGMC’s current biggest successes and how are those maintained?
Hudson: MGMC’s status as a Baldrige National Quality Award recipient and a Magnet organization are objective indicators of the highest levels of quality patient and family care, sustainable leadership and improvement systems, and dedication to monitoring and acting upon key performance metrics.
I believe that my background in immersive involvement in hospital operations and service as an outsourcing partner for health systems gives me the perspective to judge strengths and opportunities for improvement. MGMC is led by a well-qualified and effective team of leaders that have established and sustain an environment of engagement, monitor and support a culture of the highest quality of interpersonal and clinical care, and ensure the enduring financial underpinnings necessary to achieve those aims.
MGMC’s positioning as an independent regional hospital partnered with a well-regarded multi-speciality physician practice, in a university town, located at some distance from tertiary care centers, is advantageous in the current health care marketplace.
Kitchell: MGMC is highly regarded in the hospital world for consistently high quality and safety, positive patient experience, and financial stability reflected by the Malcolm Baldrige National Quality Award, the nation’s highest recognition for performance excellence and Magnet Designation, the nation’s top recognition for nursing quality. There are only a handful of hospitals in the U.S. that have achieved this. Some years ago, the MGMC Board established quality and safety as our north star, our guiding principle. It is maintained by insistence on transparency, oversight of objective performance metrics, and methodical approaches to problem-solving. MGMC’s secret sauce is its workplace culture, which takes years to develop. Objective surveys reveal high levels of engagement among the physicians, staff, and volunteers. Everyone is valued, everyone understands the importance of their work in achieving MGMC’s goals. Everyone is tasked with doing their work and improving their work.
Swenson: Our current successes include our new Behavior Health Unit. Historically we had to deny patients admission due to lack of space. We are now able to accommodate more patients of differing acuities into our facility, though we still have to turn away requests for transfers. We continue to look for new providers to treat our patients, both on an inpatient and outpatient basis.
Our other large success is the opening of our Ambulatory Surgical Center. We formed a partnership with McFarland Clinic to bring this project to fruition. Because insurance was not looking favorably on outpatient surgeries done in a hospital, as the inherent costs in a hospital were higher than in an outpatient center, which didn’t work 24/7, we made the decision to partner and build this great center.
What are the major challenges MGMC currently faces and how might you work toward developing solutions?
Hudson: The financial impact of the move of a substantial and significant insurance-supported procedures and surgeries to the new outpatient surgery center is concerning, and measures and plans to compensate for that lost income are part of the strategic planning process and the leadership’s vision for the future of the medical center. Changes in health care reimbursement, notably new national Medicaid requirements and the shortfall in proceeds from commercial payers — specifically Medicare Advantage programs — will serve as stressors as the hospital moves to grow out of the aforementioned deficit.
The move away from hospital-based care to technology-based solutions like telemedicine, mobile integrative care, and hospital-at-home, along with an emphasis on population and community health, will continue the significant change in the hospital’s mission and the government’s and payers’ expectations. Similarly, outcomes-based reimbursement and the possibility of some form of capitated payments for a set of covered lives are part of the current and future landscape. Expansion and encroachment of regional and national health care organizations will provide a competitive threat, especially if those organizations target key demographics in the hospital’s service area. I believe I am sufficiently versed in the contemplated and emerging opportunities to provide support and counsel on these, and other, issues as a member of the board.
Kitchell: The challenges for MGMC reflect challenges in health care everywhere in the U.S. The cost of health care is high for funders (individuals, employers, government), for providers (personnel, equipment, technology, facilities, supplies, pharma), and for consumers, and all involved struggle to afford it. With rising consumer expectations and our aging population, demand for services will increase. There are serious shortages in most health care jobs. Knowledge of health conditions is unfolding exponentially, prompting greater cognitive load for workers, increasing stress, and potential burnout. There is increased competition from outside the traditional health care world. These challenges are large and often outside the control of local entities; however, we can align with the Iowa Hospital Association and the American Hospital Association to develop policy and to advocate with our legislators. Locally, we can focus on what we can control. We can explore how to work smarter, how to deploy technology, how to collaborate with local interests. Best practice in governance is not to micromanage but to install great leadership, to set broad policy and direction, to ensure accountability and transparency, and to arrive at data-driven decisions.
Swenson: Our biggest current challenge is currently in Congress and has caused a government shutdown. The economy is at a standstill, and so is our financial future. The proposed changes to Medicare and Medicaid could affect our financial future through cuts to current programs and reimbursement rates. We do look at how this may affect us and our ability to provide our patients with quality care. We have to carefully look at future plans, like the “Education Center,” until we are certain of our financial future.
What would you hope to accomplish in the next term on the board of trustees?
Hudson: Execute and adapt the strategic plan with an aim to achieve the return to “in the black” financial performance. Advance investigation into workforce development and retention efforts; notably — but not exclusively — the partnership with Iowa State’s nursing program. Plan for what will provide the greatest return on investment with careful stewardship of scarce resources.
Nurture and reinforce the contribution to the health care of the communities MGMC serves, with an emphasis on social determinants of health.
Kitchell: First of all, being on the board of trustees is a team effort. It means that hospital leadership and the board of trustees convene and discuss and come to consensus about policies and solutions. As an individual, I will continue to be informed about health care issues. I will listen to the voice of the patient and their families. I will respect the expertise of our staff. I will consider the viewpoint of my fellow trustees. During the past year, the board developed a new three-year strategic plan that addresses the challenges we face. I hope to see that plan come to fruition and I will work to make that happen.
Swenson: No matter what the challenges we may face, I want to work to ensure Mary Greeley remains a quality and safe place to receive care. I strive to ensure that our employees are valued and respected, and that Mary Greely remains a great place to receive care, and a great place to work. I would work to retain our Baldridge Award, as well as our Magnet awards, as a testament to excellence as a hospital. I will work to ensure that Mary Greeley remains a good neighbor to our surrounding area. I want to keep an open dialog with our neighbors to ensure their thoughts and feelings are heard and respected.
Anything else you’d like to add?
Hudson: I met my future wife working at MGMC. Both our children were born at the hospital, and I was provided outpatient care at the Bliss Cancer Center — I’m in remission, five years after that care. I spent a month at my mother’s bedside at MGMC as a family member and patient advocate.
If elected, I promise to be responsive, responsible, and dedicated.
Kitchell: Much of this narrative has focused on the transactional nature of health care: someone gets sick, they come to the hospital, they get treated, someone gets paid. But it is so much more than that. Everyone that comes to the hospital has their own story. Some of the most important, intense aspects of our lives — good and bad — can happen in hospitals. It is a human encounter where caring and compassion matter. As a trustee, it is a privilege to be a part of that life journey. It is a privilege to be given the responsibility to sustain the asset that is Mary Greeley.
Swenson: I think the financial future of all health care stands in uncertainty right now. The budget bill that has shut down our government, has potential hardships for healthcare organizations. If Medicare and Medicaid receive the proposed cuts, that could affect the financial status of hospitals through decreased reimbursements, which affects the bottom line of available health care. The increase in insurance premiums could have a devastating effect on the ability of many to afford insurance, again, effecting hospitals. Having served on the finance committee at Mary Greeley, I feel ready to face these challenges, and find ways to adapt to theses potential hardships.